The first months with a new baby can feel like living between love and yawns. As a mom who has soothed through midnight cluster feeds and early-morning diaper blowouts, I know the tug-of-war between wanting rest now and wanting to do what’s safest and healthiest long term. The market meets that tension with an avalanche of “sleep aids” promising deeper, longer slumber. Some help in specific, time-limited ways. Some do little. Some carry real risks. This guide distills what leading pediatric sleep specialists, safety regulators, and clinical researchers say, while adding the practical, gentle-parenting wisdom many of us wish we had at 3:00 AM, including the advice on choosing a baby calming sound device that might help soothe your baby to sleep.
What “Baby Sleep Aid” Really Means
Parents often picture a pill or a gadget, but experts define sleep aids more broadly. A sleep aid can be a behavior, a product, or a substance used to help a baby or child fall asleep or stay asleep. That includes soothing routines like a warm bath and book, devices like white-noise machines or swaddles, and substances like melatonin or antihistamines. Pediatric sleep medicine groups emphasize that the most effective, safest “aids” are behavioral: consistent routines, predictable schedules, sleep-conducive environments, and addressing medical contributors when present. The American Academy of Sleep Medicine’s Choosing Wisely recommendations state plainly that sedative-hypnotic medications should not be the first-line answer for children’s insomnia and that families should start with behavioral strategies rooted in sleep hygiene and caregiver-led interventions.

The Truth From Sleep Experts: Start With Behavior, Not a Bottle or Box
When a child struggles to sleep despite a good opportunity to do so and shows daytime effects like crankiness, attention issues, or school difficulties, pediatricians call it insomnia. Expert groups urge families to look for contributors before reaching for a product. That means screening for obstructive sleep apnea, restless legs linked to iron deficiency, eczema itch, reflux, pain, anxiety, depression, ADHD, or autism-related sleep challenges. Only after addressing those factors should families consider add-ons.
Behavioral approaches have the strongest safety and effectiveness profile in childhood. Routines of about 20 minutes including a calming bath, a short story, a lullaby, or gentle massage improve infant sleep in clinical studies, especially when parents repeat them steadily every night. Bedtime fading helps when a child fights sleep by starting a bit later—when the child is naturally drowsy—and then moving earlier over several evenings. Daylight exposure in the morning supports the internal clock, while dim, warm-toned light in the evening protects melatonin release. These modest changes stack up quickly and, over days to weeks, teach babies the rhythm of night and day.
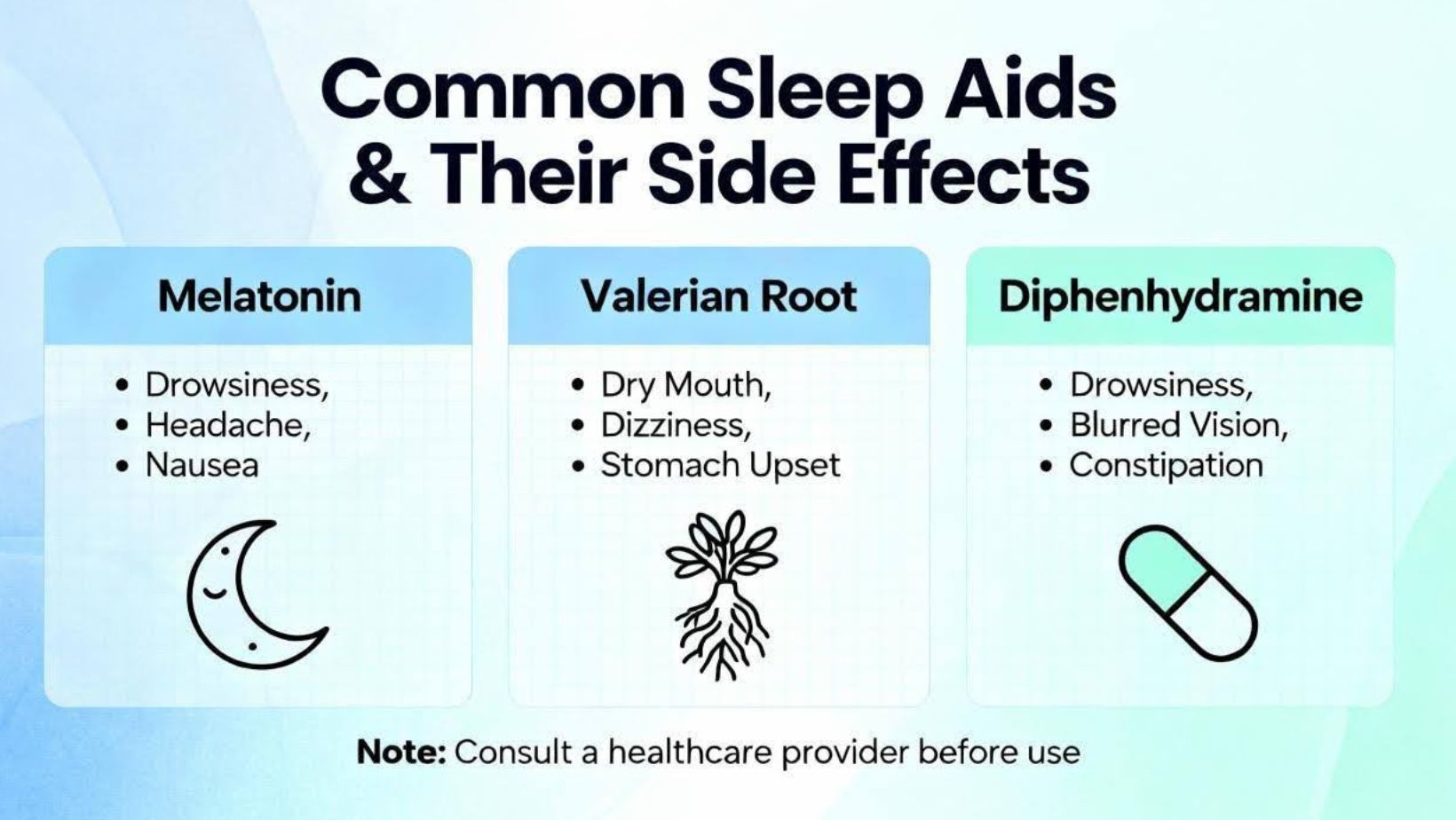
Common Sleep Aids and Their Side Effects
Sedating Medicines Are Not First-Line and Carry Real Risks
Specialists caution that most sleeping pills adults use are not approved for pediatric insomnia. Benzodiazepines, “Z-drugs,” sedating antihistamines, and antipsychotics can cause next-day grogginess, slowed thinking and reaction time, agitation in some children instead of calm, tolerance and dependence with repeated use, rebound insomnia, and potential respiratory depression in vulnerable patients. Pediatric guidance flags diphenhydramine in particular. While parents know it as an allergy medicine, the drowsiness is a side effect, not a sleep cure. Tolerance develops within days, lingering sedation can impair reflexes long into the next day, and roughly a tenth of kids act wired instead of sleepy. Under two years old, potential risks are serious enough that pediatricians advise against it for sleep. Across the board, experts recommend avoiding antihistamines and other sedatives as a routine sleep fix, and reserving any medication for carefully selected, short-term cases under medical supervision.
Melatonin Helps Some Older Kids, But Quality and Dosing Are Problematic
Melatonin is a hormone that signals the brain that darkness has arrived. In older children and teens with delayed internal clocks, careful timing of a low dose can shift the body’s schedule earlier and shorten the time it takes to fall asleep. It is not a sedative and is not a substitute for routines or good sleep hygiene. There are two big concerns. First, product quality is inconsistent. Investigations reported that many melatonin gummies marketed to children contain far more or far less melatonin than labels claim, with some serving sizes reaching levels dozens of times higher than what pediatric sleep specialists consider a reasonable starting dose. Second, exposures and accidental ingestions have surged, with hundreds of thousands of reports to poison control over the past decade, most mild but some requiring hospital care.
If a clinician recommends a brief trial in a specific situation—such as delayed sleep phase in a teen or in some children with autism or ADHD—experts suggest starting with the lowest effective dose, typically around 0.5 to 1 mg about 30 to 90 minutes before the target bedtime. Most children who benefit do not need more than a few milligrams. Families should treat melatonin as a short-term bridge while they strengthen routines, choose a third-party–tested product rather than candy-like forms, lock it away from little hands, and stop if side effects like morning sleepiness, headaches, very vivid dreams, or increased nighttime urination appear. For infants, specialists do not recommend melatonin.
Herbal and Mineral Supplements Lack Pediatric Proof
Chamomile is beloved in adult sleep teas and some studies in adults associate it with shorter time to fall asleep and fewer night wakings. There are no pediatric trials showing safety and efficacy for sleep. Magnesium has an “uncertain association” with sleep outcomes even in adult studies and has not been evaluated as a sleep aid in children. Cannabidiol and tetrahydrocannabinol raise particular concerns because of developing brains; pediatric policy statements caution that exposure in youth is linked to difficulties with thinking, memory, and learning. Expert consensus today is clear: do not use cannabis-derived products as sleep aids in children or adolescents, and avoid giving infants any supplements or herbals unless a pediatrician specifically recommends them.
White Noise Helps Some Babies—Volume and Distance Matter
A small study in newborns found many fell asleep more quickly with white noise compared with those without it, and many families report fewer disruptions when background household sounds are masked. However, safety depends on sound level and placement. Pediatric guidance recommends keeping nursery sound levels no louder than a quiet conversation and placing machines at least about 7 feet from the crib. Measurements published in Pediatrics found that many infant white-noise machines can exceed safe levels at close range or high settings. Prolonged exposure to loud sound may harm hearing and auditory development. If you use white noise, keep the volume low, the device far from the crib, cords secured and out of reach, and consider using a timer or turning it down once your baby is asleep. Watch for dependency as your child grows and plan to phase it down gradually.
Swaddles, Weighted Sleepwear, and the Allure of “Deeper Sleep”
Some babies settle better when their arms are lightly contained because it dampens the startle reflex. Swaddling can be used safely if babies are always placed on their backs, the wrap is snug at the torso but allows hip movement, and parents stop swaddling the moment a baby shows signs of rolling. Prone swaddling, tight wrapping across the chest, overheating, and any fabric near the face increase risk. Weighted blankets, weighted swaddles, and devices claiming to induce deeper sleep are not recommended for infants because they may blunt natural arousal and raise suffocation risk. Safety organizations emphasize that a young infant’s ability to wake and cry is protective; products that push “longer, deeper sleep” can undermine that protection.
Inclined or Rocking Sleepers Are Off the Table
Tragic deaths linked to inclined sleeper products prompted recalls and spurred new rules requiring all infant sleep products to meet crib and bassinet safety standards. The safest infant sleep surface remains simple: flat, firm, and bare, with a fitted sheet, and the baby placed on the back for every sleep. Swings, bouncers, car seats, and hammocks are not safe for unsupervised sleep; if a baby dozes in one, transfer to a firm, flat mattress as soon as possible.
Pacifiers and Transitional Objects
Pacifiers soothe through sucking, may help reduce feed-to-sleep associations, and some observational research suggests they are associated with a lower risk of sudden infant death. Use a size that matches your child’s age, clean and replace regularly, never tie a pacifier around a neck or attach it with cords, and do not reinsert it after a baby falls asleep. Many safe-sleep guidelines advise keeping cribs bare of soft toys and loose objects in infancy. As toddlers move to their own bed, a small, safe comfort object can help with separation anxiety and bedtime jitters.
Quick Comparison: Benefits, Risks, and Expert Take
| Aid or Product | What It Does | Potential Benefits | Key Risks or Side Effects | Age Notes | Expert Take |
|---|---|---|---|---|---|
| Melatonin | Signals body clock timing | Shortens sleep-onset latency in specific cases | Morning grogginess, vivid dreams, dosing variability, poisonings; unknown long-term effects on puberty | Not for infants; use short-term in older children with guidance | Consider only after behavioral steps, lowest dose, third-party tested |
| Antihistamines (e.g., diphenhydramine) | Causes drowsiness as side effect | May make some kids sleepy acutely | Tolerance in days, paradoxical hyperactivity, next-day impairment; safety concerns under two | Avoid under two; avoid routine use | Not recommended as a pediatric sleep aid |
| White Noise | Masks disruptive sounds | Faster sleep onset for some; fewer arousals in noisy homes | Excess noise exposure, dependency if overused | All ages with safe setup | Keep below about 50 dB; place about 7 ft away; cords secured |
| Swaddle | Dampens startle reflex | Calmer settling in early months | Overheating, restricted breathing if improper; unsafe once rolling begins | Newborns until rolling signs | Always back-sleep; stop at first rolling attempts |
| Weighted devices | Add pressure for “deeper sleep” | Marketing claims of longer sleep | May blunt arousal; suffocation risk | Not for infants | Avoid in infancy |
| Inclined sleeper/rocker | Holds baby at an angle | Appears soothing | Asphyxiation risk; recalled products linked to deaths | Infants | Unsafe for sleep; use flat, firm, bare surfaces |
| Pacifier | Soothing via non-nutritive sucking | May reduce SIDS risk; portable | Dependency, need for replacement, hygiene issues | Infancy and beyond | Use safely; never attach with strings; do not reinsert once asleep |
| Chamomile, magnesium, CBD/THC | Herbal/mineral/cannabis agents | Adult data suggest possible calm with chamomile | Lack of pediatric evidence; developmental risks with cannabis | Children and teens | Do not recommend for pediatric sleep without clinical indications; avoid cannabis products |
Purchasing and Care Tips When You Do Use Aids
Parents are not failing when they reach for tools. The key is choosing and using them safely. For any supplement, select brands that publish independent third-party testing and list exact ingredients and amounts; avoid candy-like gummies with cartoon marketing and store all supplements locked away. For sleep machines and night gadgets, prefer models with volume caps and clear decibel specifications, keep them far from the crib, and secure cords and cables outside the sleep area. For wearable products, choose breathable fabrics that keep the face and head clear, follow room temperature guidance to avoid overheating, and stop immediately when a baby meets a safety milestone like rolling. Register every product with the manufacturer so recall notices reach you promptly, and check for updates from safety agencies and your pediatrician’s office. Cleaning and replacement schedules matter, too; pacifiers and nipples degrade with use and require routine sanitation and frequent replacement.
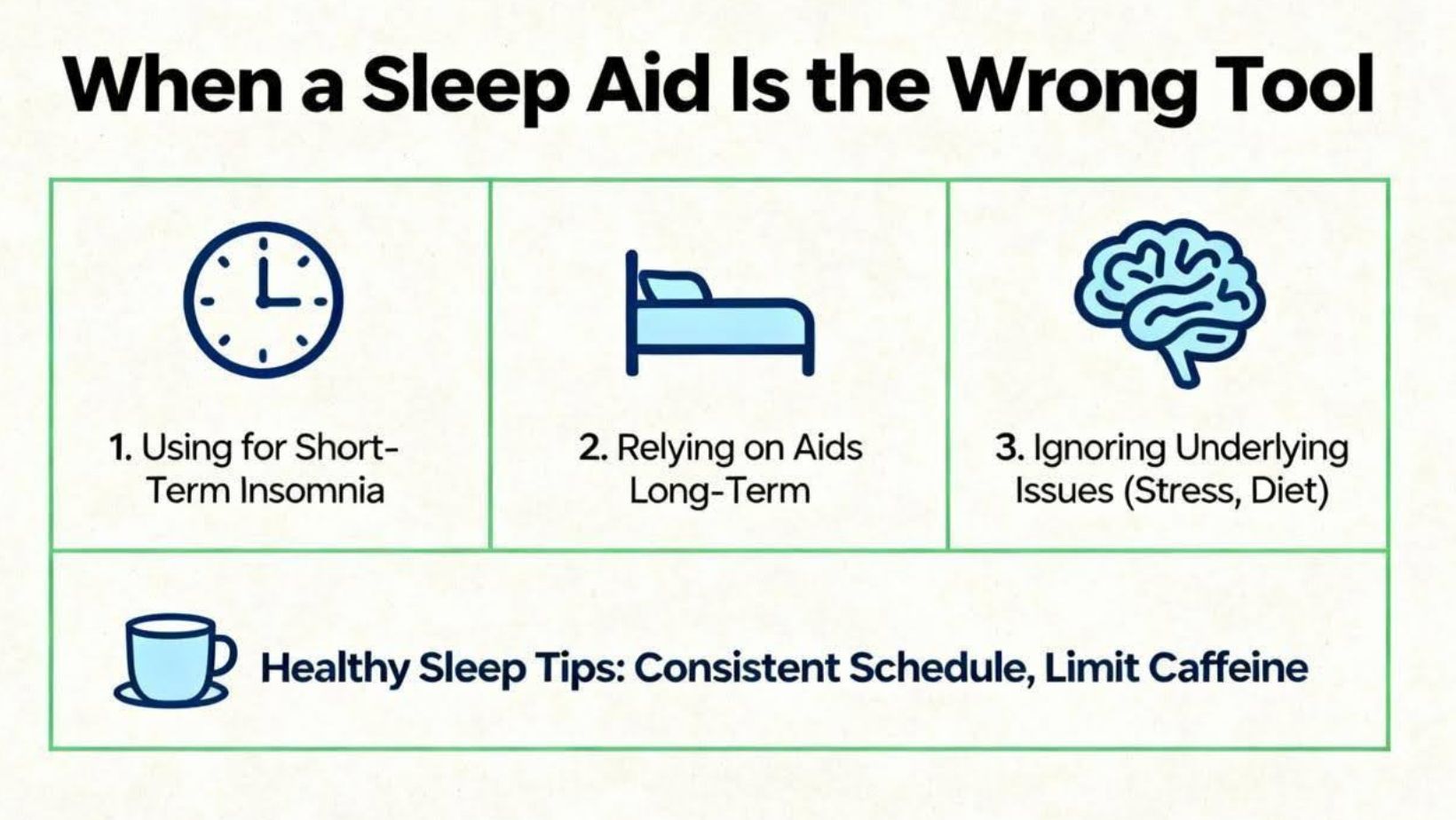
When a Sleep Aid Is the Wrong Tool
If your child snores most nights, breathes through the mouth with pauses, sweats heavily or works hard to breathe during sleep, or wakes persistently with leg discomfort or kicking, a sleep study may be needed to check for obstructive sleep apnea or movement disorders. If your child lies awake for hours despite a sound routine, talk with your pediatrician about anxiety, depression, or ADHD screening. Iron deficiency can drive restless sleep and is treatable. In infants, reflux rarely justifies inclined sleep; flat, back sleep actually protects the airway. Medically complex babies coming home from the NICU should follow the same safe-sleep basics, with special instruction on routing tubes and wires safely out of the crib.
Gentle, Evidence-Backed Alternatives I Trust as a Mom
Families do not have to choose between attachment and evidence. Skin-to-skin time in the early weeks helps babies regulate and cry less. A simple, repeated bedtime routine, the same sequence at about the same time, becomes an anchor that babies quickly recognize. If your baby resists an early bedtime, try bedtime fading by beginning the routine slightly later when drowsiness is more reliable and then move it earlier by small steps over several nights. Morning outdoor light resets the clock, and dimming bright and blue-leaning light in the hour before bed protects night melatonin release. Gentle, brief infant massage has been linked to easier bedtimes and fewer night wakings in small studies; if you try it, keep it short and soothing. Rocking and walking can be a bridge on hard nights, and with practice you can set your baby down drowsy rather than fully asleep to build self-settling gradually. Room-sharing keeps babies close without bed-sharing risks, and side-car cribs designed to attach securely to the adult bed can ease access for breastfeeding, particularly in postpartum recovery, while preserving a separate, flat sleep surface.
The Bottom-Line Takeaway
The safest, most reliable path to better sleep in infancy and childhood looks ordinary: back to sleep on a flat, firm, bare surface; a calm, consistent bedtime routine; morning light and evening dimness; and addressing medical or developmental contributors with your pediatric team. Sleep aids can have a place, but they are not a cure-all. Some, like white noise used softly and at a distance, can help when used thoughtfully. Some, like melatonin, help a subset of older children when dosed conservatively for a short time under medical guidance. Others, like sedating antihistamines, cannabis products, weighted infant wearables, and inclined sleepers, carry risks that outweigh benefits. As a seasoned mom, I know the pull of a quick fix at 2:00 AM. As a gentle parenting advocate, I also know that small, steady changes add up. With patience, safety-first choices, and the right kind of support, your family can find a rhythm that honors your baby’s biology and your need for rest.
Short FAQ
Is Melatonin Safe For My Toddler?
Melatonin can help older children who fall asleep very late by nudging the body clock earlier, but it is not a sedative and not a first step. If your pediatrician recommends a short trial, start low—often around 0.5 to 1 mg about 30 to 90 minutes before bedtime—pair it with a solid routine, choose a third-party–tested product, and lock it away. Stop if you see side effects such as morning grogginess or headaches. It is not recommended for infants.
Are White-Noise Machines Safe In The Nursery?
Yes when used thoughtfully. Keep the volume low, roughly at or below a quiet conversation, place the device about 7 feet from the crib, secure cords out of reach, and avoid running it around the clock. If your baby seems distressed by the sound or if you find yourself turning it up to drown out normal home noise, turn it down or off.
Do Weighted Sleep Sacks Make Babies Sleep Better?
Weighted infant sleepwear is not recommended. It may blunt natural arousal, which is protective in young babies, and can raise suffocation risk. For safe soothing, use a standard swaddle only until rolling begins and always place your baby on the back to sleep.
Can I Give My Child Benadryl To Sleep Before A Big Day?
Pediatric experts advise against using antihistamines as sleep aids. Children can become tolerant within days, many have next-day sedation or, in some cases, paradoxical hyperactivity, and there are safety concerns in younger children. Focus on routine, timing, and environment instead.
How Do I Wean A Pacifier Without Wrecking Sleep?
Start when your child is well and routines are steady. Begin with one sleep a day without the pacifier, add extra soothing through touch and voice, and keep everything else predictable. If your child is older and in a bed, consider a new comfort object and rehearse the new routine together during the day. Expect a few tough nights, then consistency pays off.
Are Smart Bassinets Safe?
Smart bassinets that keep babies on a flat, firm surface and follow safe-sleep guidance can be used for supervised settling. They should not replace the safety basics. If motion is used, keep it gentle, avoid prolonged rocking through the night, and transition to a static sleep surface as early as is practical.
References
American Academy of Sleep Medicine, Choosing Wisely guidance on pediatric insomnia and first-line behavioral strategies.
American Academy of Pediatrics, HealthyChildren guidance on melatonin use, poisoning trends, and screen-time effects on sleep.
JAMA and academic reports on melatonin product mislabeling in child-marketed gummies and supplements.
Consumer Product Safety Commission rules requiring infant sleep products to meet crib and bassinet standards and recall summaries of inclined sleepers.
Pediatrics research on infant sound machines and nursery sound levels, and clinical advice on safe use of white noise.
Parenting Science summaries of bedtime routines, bedtime fading, swaddling safety, infant massage, white noise evidence, and skin-to-skin care.
UPMC HealthBeat and Sleep Foundation overviews of white noise benefits and practical safe-use guidance.
Pediatric Associates of Richmond review of melatonin dosing, magnesium and chamomile evidence gaps, and cannabis cautions.
BASIS guidance on infant arousability, safe room-sharing, and risks of products claiming “deeper sleep.”
Children’s hospital safe-sleep guidance for medically complex infants, including advice on transferring from devices to flat, back sleep and safe routing of equipment.